Just one year ago, Optum gauged the average private payer denial rate at 12%.
More recently, a survey of 516 hospitals in 36 states bumped it up to 15%. Providers are not surprised. Research published in Revenue Cycle intelligence reports that 75% of the healthcare organization executives they surveyed have noticed that denials are getting more frequent.
Considering denials can consume up to five percent of net patient revenue and deplete revenue by hundreds of thousands of dollars, it’s no wonder that denials are a top revenue cycle focus for MSO and physician group revenue cycle executives.
As Aaron Wesolowski, the AHA’s vice president of research strategy explains,
"What we've seen in the last few years — particularly since the pandemic — is a really drastic increase in the rate of denials, as well as the broad application of prior authorization requests. This has had an impact on hospitals' ability to provide care..."
Organizations manage denials either manually with in-house staff, by outsourcing to a third party, using denials management software, or a combination of these.
A robust denial management program can drop your claim denial rate to 5%, the industry’s benchmark. Use this article to evaluate your denials management system’s efficacy, whether it’s time for denial management software, and what you stand to gain with more aggressive denials processes.
What is denial management in medical billing and RCM?
Denial management is the process of preventing, investigating, analyzing, and resolving denied insurance claims. It aims to optimize the revenue cycle by reducing denial rates, improving clean claim submissions, and enhancing overall financial performance. Healthcare organizations need a robust denial management process to ensure payers are not taking advantage of them.
Healthcare organizations lose hundreds of thousands, even millions, every year because of denied healthcare claims that may have been prevented with strong denial management processes.
For instance, according to “The Change Healthcare Revenue Cycle Denials Index,” the average cost to rework a claim ranges from $25 to $117. If you decide to appeal 100 denials per month, your organization invests $2,500 to $11,700 in this effort. By proactively managing denials, healthcare professionals can focus on delivering quality patient care while ensuring timely and accurate reimbursement from payers.
Denial rework and denial appeal support
In healthcare revenue cycle management, denial management involves two critical processes: denial rework and appeal support. Denial rework addresses claims rejected due to internal errors, focusing on correcting coding mistakes, updating documentation, and resolving administrative issues before resubmission.
Appeal process support, conversely, challenges payer decisions by formally contesting claim denials. This process requires preparing comprehensive documentation, referencing policy guidelines, and presenting a compelling case for claim reconsideration. While denial rework targets internal operational improvements, appeal support advocates for claim approval through strategic administrative intervention and possibly legal action.
Both approaches are essential strategies for maximizing reimbursement via denial management.
Take a quick, self-guided tour through a powerful denial and contract management system:
The denial management process
The denial management process can return meaningful revenue if handled correctly. Effective denial management involves the following steps:
Step 1: Examine all aspects of denials
The first thing provider groups and management services organizations need to do is examine where denials occur. You need a clear picture of what types of denials occur most frequently and which payers are the most likely to deny which procedures. Gathering data on what facilities, providers, payers, and procedures result in the most common denials uncovers not only where your errors are occurring but also where payers could be making mistakes. Pinpointing root causes prompts staff to rectify them.
Step 2: Analyze reasons behind denials
On the provider end, behind these claim denials lie coding errors, missing data, late submissions, out-of-network care, lack of prior authorization, and lack of medical necessity. Robust denial management software covers all of these areas. The top reasons for denials according to Optum research are:
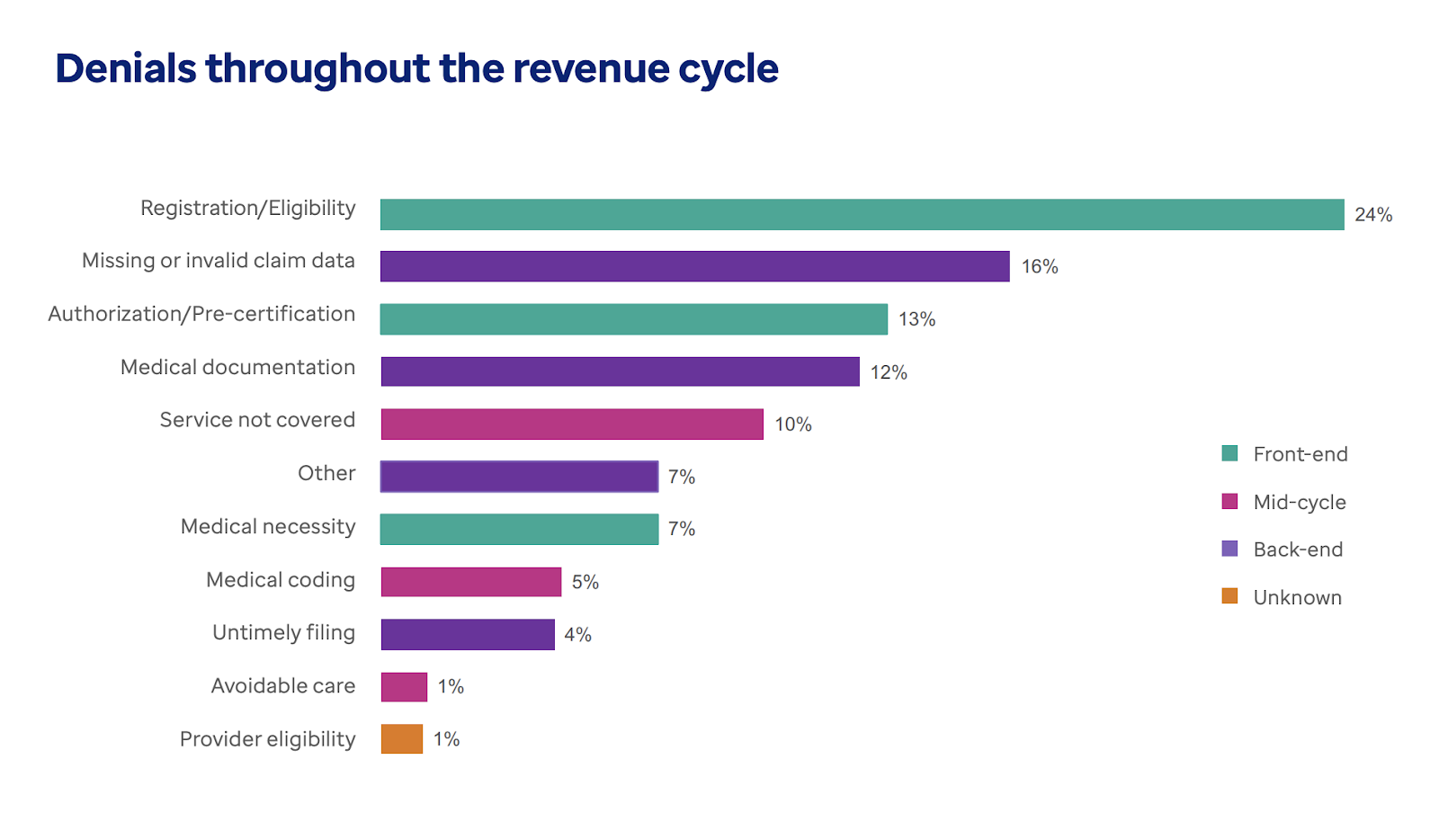
Source: Optum 2024 Revenue Cycle Denials Index
By identifying the causes, you can develop strategies to prevent similar denials. Denial management software pinpoints the issues behind your denials so that you can adjust your workflow processes to prevent them.
Step 3: Categorize denials
The next step in the denial management process is categorizing denials to develop targeted strategies for preventing future denials of a similar nature. Denials can be categorized by specific causes, such as:
- Prior authorization: If prior authorization is required for the services given or prescribed, a claim may be denied without it.
- Incomplete information and coding errors: Missing information and incorrect coding can result in a denial.
- Claim filing delays: Payers have time frames for submitting claims. If you miss this deadline, the claim can be denied.
- Coverage: If a claim is submitted for a service not covered by insurance or the payer determines that there is a lack of medical necessity, it can result in a denial.
Other categories to consider are the types of claim denials, such as:
- Soft denials: A temporary denial that does not require an appeal and that may be paid if your healthcare organization corrects the issue
- Hard denial: A denial that results in lost revenue and requires an appeal
- Preventable denial: A hard denial caused by avoidable reasons, such as code errors or insurance ineligibility
- Clinical denial: A hard denial in which a claim is not paid due to a lack of medical necessity
- Administrative denial: A soft denial in which your organization is told by the payer precisely why the claim was denied
After categorizing the denials, you'll need to assign departments/teams for corrective actions. Not all denials are equal, and categorizing denials can help teams determine which are most pressing. No team has unlimited resources, so this step can also help you use your staff and resources wisely.
Step 4: Marshal supporting facts and documents and resubmit
After identifying the reasons for the denial and categorizing it, you can correct the errors or address the issues that caused the denial in the first place and then resubmit the claim for payment. Because so many denials are reversible, this step is critical to increasing revenue rather than losing money that may rightfully be owed to your organization.
Appeals can be won. Even though 67 percent of denials are recoverable, the majority are never resubmitted. Clearly healthcare organizations simply do not have either the staff or systems to handle denials effectively. When providers are overwhelmed, payers benefit.
Step 5: Recover denied claims
Provider organizations most eager to stem their denials may need to use staff members or outside denial recovery services to directly connect with payers via phone and email. Some denial management software employ recovery services experts to negotiate with payers. They support their demands with the data and insights generated by the denial management software.
Step 6: Track results
The fourth step in the denial management process is to develop a tracking mechanism to monitor the progress of resubmitted claims. When you track and stay within timelines, payers cannot deny due to missing a deadline. Further, if they miss a deadline, they are subject to penalties, a fact you can remind them of should they start dragging their feet on your appeal.
Step 7: Build a preventative mechanism
With clear insight into the missteps clinicians and administration make that prompt denials, as well as the payer issues, prepare a checklist of the top reasons for denials. Work with your team to implement strategies to prevent these common denials from occurring.
Monitoring future claims before submission
Some revenue cycle managers have dropped their denials rate by using RCM software that features a predictive analytics tool. Because appealing a claim can cost your organization between $25 and $117, preventing a denial should be a first step.
Predictive functionality understands which of your claims are most likely to result in denials. It ultimately improves financial outcomes for healthcare organizations. These tools utilize data analytics, machine learning algorithms, and historical data to detect patterns and trends and then accurately predict the likelihood of claim denials before submission.
With the types of high-denial-risk claims flagged, you can create a workflow for staff to include all required aspects for that payer. This list should include everything that got similar claims approved with the payer in the past. A proactive approach addresses the common billing and coding issues involved with the procedure, physician, or payer.
Benefits of managing denials in a healthcare organization
There are tremendous benefits to managing denials in your healthcare organization.
Improved clean claims rate
While a 95% clean claims rate is excellent, according to HFMA, physician groups and management services organizations should strive for a clean claims rate of 98 percent. As mentioned above, denied claims rack up administrative costs, staff working hours, and payment delays.
Increased net revenue collection
Another advantage of proactively managing denials is the potential for net revenue increase. Paying $25 to $117 for each rework or denial appeal adds up. By addressing denials proactively, organizations can recoup a substantial portion of potential revenue that would otherwise be lost. Timely resolution of denials helps maintain consistent cash flow, supporting operational expenses and growth opportunities.
Enhanced patient experience and loyalty
In addition to the financial benefits, managing denials can enhance patient experience and loyalty. Denied claims frustrate patients who are anxious to get the care they need. Only satisfied patients drive the word-of-mouth referrals critical to increasing your patient base.
Reduced revenue leakage
With up to 80% or more of denied claims considered recoverable, aggressive management can minimize financial losses and stabilize cash flow. An optimized revenue cycle with controlled loss impresses investors, lenders, and buyers.
Decreased administrative burden
By streamlining denial management processes, organizations can reduce the time and resources spent on resolving claims issues.
Improved operational efficiency
Analyzing denial patterns and implementing targeted interventions can lead to process improvements across the revenue cycle. Better systems lead to happier employees.
In an environment where payers seem to have all the power, it makes sense to invest in capturing these advantages.
Best practices and strategies for denial management
With the increasing complexity of healthcare reimbursement and coding requirements, effective denial management requires significant input from teams. More teams are looking to software for support.
Leverage denial management software
A healthcare staffing shortage and expertise deficit have pushed many physician groups and management services organizations to use software to tackle denials and appeals.
Valerie DeCaro is the revenue cycle management vice president at DOCS Dermatology. With dozens of locations hosting over 150 providers, DOCS works hard to standardize and simplify their revenue cycle. DeCaro laments how healthcare has lagged in the adoption of technology. One of the biggest problems management services organizations like her face today is:
“the lack of catch-up in healthcare around using automation and technology. We have many archaic workflows, and we still use fax machines regularly. Some practices still operate on paper systems. We're not anywhere close to where other industries are. You can check in at an airline on your phone, pay for your bag, print your tag, do all of that before you even get to the airport.”
The rate of change in the healthcare industry juxtaposed with a debilitating revenue cycle management staffing shortage has prompted organizations to depend more on technology to get critical RCM administrative tasks completed.
Healthcare leaders are unanimous in urging providers to adopt technical solutions.
In “The gathering storm: the uncertain future of US healthcare,”, healthcare leaders at the renowned healthcare consulting firm McKinsey explain,
“The imperative for companies that seek to thrive in coming years will be scaling up innovations much more quickly than they currently do.”
Resilient providers are overcoming hesitancy and investing in revenue cycle technology.
Despite concerns about time, budget, and capacity, healthcare leaders can rest assured that third-party solution partners have made efforts to ensure seamless integration with your current EMR, billing, and other systems. Understanding healthcare organization’s limited time and budget, partners aim to make the experience as "touchless" for healthcare leaders as possible. Data seamlessly flows through your existing systems, and the partner offers comprehensive onboarding and support at every step.
Synergize software with revenue recovery services
Fully comprehensive denial management programs use both software and denial management experts to initiate direct payer engagement. Seasoned professionals not only know how to overcome payer stonewalling tactics, but they clearly signal your commitment to overturning incorrect denials. Their deep expertise in payer reimbursement methods and appeals processes improves denial overturn rates and shrinks denial backlogs to quickly generate cash collections. They aim to ensure payers address your claims fairly and reliably, helping you secure the reimbursements you deserve.
Conduct performance audits
According to suggestions from AHIMA, continually performing audits on things like remittance advice reviews, zero payment claims, registration, and insurance verification quality can improve denials and appeals rates.
Collaborate
Your denial management team should not be a one-person endeavor. Establishing a multidisciplinary team of key members from various departments such as registration, patient financial services, nursing, health information management, and information technology can help you put solutions in place and track developments to alleviate bottlenecks in the processes and identify the root causes of these denials. Collaborating with payers to resolve denial claims can also ensure a more efficient process.
Another form of necessary collaboration is staff training. Training staff to stay current on best practices will help ensure that you are mitigating denials as much as possible.
Be mindful of statistics and trends
Knowing what’s “normal” in today’s healthcare landscape helps keep you on track. As mentioned above, today’s 15% denial rate reflects an increase of 67% from 2016’s rate of 9%.
These numbers have more meaning when you break them down by your specialty. Medscape surveyed 17,461 U.S. clinicians representing more than 30 specialties. These are just 10 of the denial averages:
- Plastic surgery: 28 percent
- Emergency medicine: 22 percent
- Radiology: 20 percent
- Orthopedics: 18 percent
- Oncology: 16 percent
- Gastroenterology: 16 percent
- Dermatology: 15 percent
- Internal medicine: 15 percent
- Family medicine: 14 percent
- Ophthalmology: 13 percent
Comparing your denials numbers to industry averages let you know when you need to double-down on your denials management system. Showing divergence from industry averages also helps you get buy-in from peers and managers.
Stay on time
When it comes to denials, time is of the essence. It's crucial to comply with both the initial claims filing as well as appeals deadlines set by insurance companies. Keep staff on track with a documented process. Keep in mind, too, that payers must conform to deadlines. When they don’t they are subject to penalties.
Solutions to denial management when your staff is constrained
Healthcare revenue cycle managers and management service organizations would love to unleash all of the solutions mentioned above. When you’re struggling just to get patients scheduled and in the door, however, denials become a secondary consideration.
Denial management software
Denial management software assists healthcare providers in navigating and resolving claim denials from insurance companies and other payers. Aiming to improve revenue cycles and maximize reimbursement, this software identifies, tracks, and even appeals these claim denials in some cases. These software solutions offer real-time denial tracking, data analytics, customizable workflows, and integration with existing electronic health record systems.
Because multiple code systems are used in the claims process, there are many opportunities for mistakes. Even a single typo can result in a claim being denied. Denial management software assists you in properly coding your claims and understanding the meaning of a denial code if a claim is denied.
Denial management software proactively prevents many errors, a critical contribution if you are short on staff. By leveraging technology to automate tasks within the denial management process, your team accomplishes more. The denial recovery services your software company offers help ensure you maximize denial overturns without having to add house staff.
Outsourced denial management services
Another denial management solution that may be helpful when you have limited staff resources is to outsource denial management tasks to third-party providers. Many healthcare organizations go this route, and you can use the outsourced party's expertise and resources to identify and address issues quickly and effectively when you do not have a team in-house.
TruBridge
TruBridge is a healthcare revenue cycle management company that provides a comprehensive suite of services, including outsourced denial management services. The company's denial management program is designed to identify and eliminate the causes of denials to increase reimbursements.
With this outsourced program, TruBridge's denial management experts first work with you to analyze your claims data and then categorize and prioritize your denials. Then TruBridge performs an on-site assessment and remediation of your organization to determine the root causes of your denials, review your workflows, and implement best practices to prevent denials.
TruBridge also offers ongoing tracking and surveillance of your systems and workflows to fine-tune processes and ensure everything works as intended.
Savista
Another company that provides outsourced denial management services is Savista. Savista is a healthcare technology and services company specializing in revenue cycle management services. The company's denial management program is an outsourcing option that also aims to simplify the denial management process for healthcare organizations. Savista's denial management experts use a combination of technology and human expertise to identify the root causes of denials, develop processes within the company to avoid denials, and create an effective appeal process. According to their website, Savista was even able to recover $20 million for their client, Southwestern Health System.
Denial management software solutions
To address the rising concern regarding claim denials and their challenges, a growing number of companies are focusing on healthcare denial management and providing specialized services and solutions designed to help you manage denials effectively.
MD Clarity
MD Clarity’s RevFind targets one of the major causes of front-end denials: eligibility and registration. Because it integrates rates, terms, and contracts from hundreds of payers, RevFind has one of the highest accuracy rates in the industry.
Leveraging claim and remittance data from your practice management system or clearinghouse, RevFind’s reporting interface enables in-depth analysis of denials down to individual claim lines. Users can examine and generate reports on denials across multiple dimensions, such as denial codes, procedure codes, facilities, providers, and insurers. This flexibility allows team members to create customized reports that provide the information they need, surpassing standard reporting. Root cause identification and trend analysis allow you to prevent denials before they occur.
By equipping more staff with the necessary data to tackle denials and file appeals effectively, RevFind enhances your team's ability to optimize cash flow.
RevFind’s workqueue feature streamlines denial management by automatically distributing denied claims to the relevant team members. This assignment process can be customized based on various criteria, including denial type, insurance provider, healthcare provider, facility, or other relevant factors. Team members can easily mark claims that are prepared for appeal and generate comprehensive reports for submission to payers, facilitating reprocessing. This automation reduces confusion and fosters a more proactive and efficient appeals process.
Change Healthcare / Optum
Change Healthcare was acquired by Optum (a United Healthcare Group property) in 2022. It publishes what is now The Optum Healthcare Denial Index mentioned throughout this guide. Optum typically serves large hospitals and healthcare systems.
The Denial Index is a valuable resource for healthcare organizations looking to decrease their denial rates as the report provides insights into denial trends, denial causes, and avoidable denials. The Denial Index also provides best practices on proactively managing denials and answers frequently asked questions from the healthcare community about denials. Optum offers a lot of value for the continual development of the denial management process.
Vyne Trellis
Another company that is focused on healthcare denial management is Vyne Trellis. While Change Healthcare provides relevant insights for a range of healthcare providers, Vyne Trellis is focused specifically on dental practices. The company provides a suite of denial management solutions designed to help dental practices manage denials more effectively, such as their eligibility tool that allows dental professionals to verify patient benefits quickly and in real time. They also offer claim denial support to help with rejection reasons and status updates.
The cost of these solutions for managing denied claims
When it comes to denial management solutions, the costs can vary depending on the provider. According to Dental Claim Support, Vyne Trellis denial management services, for example, charge $99 per month per practice location, which adds up to nearly $1,200 per year.
However, TruBridge, Savista, and Change Healthcare have not disclosed their pricing information for their denial management services, which is a common practice among software sellers and service providers. In general, denial management software is priced on specific features needed and patient encounter volume.
If you're interested in obtaining current pricing for those solutions, you will need to contact each company directly.
Establish your end-to-end denial management program with MD Clarity
Claim denials are a huge burden for healthcare organizations. Staffing, high denial volume and varying commitment to technology improvements are all fueling the rise in denials.
Denials management software can do much of the work for you.
MD Clarity's RevFind is an advanced software solution that can automate processes in the denial management cycle. It streamlines underpayment detection, denial management, and contract optimization by analyzing your payer contracts to reveal hidden revenue opportunities. With all your contracts centralized in one secure platform, you can quickly identify underpayments, address denial patterns, and gain charge-level insights into reimbursement trends. RevFind empowers healthcare organizations to minimize denials, maximize revenue, and negotiate stronger payer contracts with confidence.
Provider organizations that want to execute on the insights from denial management software can inquire about MD Clarity’s Denial Recovery Services. Our seasoned professionals make the connections with payers that demonstrate your determination to collect overturned denials. They are experienced in how to stop payers from stonewalling and get you appropriate reimbursement.
To see how MD Clarity offers RevFind to finesse and empower denial management and recovery experts to make the connections that get you paid, schedule a demo today.
FAQs
Get paid in full by bringing clarity to your revenue cycle


.avif)
.svg)
.svg)