With denials reaching 15% for the average provider, healthcare organizations and management services organizations need a solid denial management process to remain viable and grow. Denials are a top revenue cycle focus for MSO and physician group revenue cycle executives year after year. Only a solid denial management process will bring denial rates down to 5%, the industry’s benchmark.
These seven key questions help you evaluate the maturity of your denial management process. How will you score?
❑ Are we accurately identifying and categorizing denials by type and root cause?
❑ Do we have a robust system for analyzing denial patterns and trends across different payers and service lines?
❑ How effective is our current process in preventing recurring denials?
❑ Are we leveraging data analytics and predictive modeling to proactively identify potential denials?
❑ What is our success rate in appealing denials, and how does it vary by payer and denial type?
❑ How efficiently are we resolving denials, and what is our average time to resolution?
❑ How well are we tracking and quantifying the financial impact of our denial management efforts, including low-dollar write-offs?
By regularly assessing these aspects of your denial management process, you can identify areas for improvement and optimize your revenue cycle management.
Review this article to evaluate your denial management system’s efficacy, determine whether it’s time for denial management software, and what you stand to gain with more aggressive denials processes.
What is a denial management process?
A healthcare denial management process is a systematic approach to identifying, analyzing, and resolving claim denials from payers. A solid process fuels a healthcare organization’s denial prevention efforts.
Your denial management process should involve a comprehensive workflow that includes:
- detecting denied claims
- investigating the root causes of denials
- delegating work
- correcting errors
- resubmitting claims
- recovering overturned denials
- implementing strategies to reduce future denials
Manual v. automated denial management
Despite the denial management automation software tools in the market today, in a recent survey of 350 healthcare finance and revenue cycle leaders, 62% report that no part of their denial management system is automated. Some organizations establish dedicated denial management teams, while others distribute responsibilities across existing staff or outsource to third-party services.
Automation of this part of the revenue cycle lags other areas for good reason. In the great digitization of healthcare, software developers started with the most serious revenue roadblocks which included:
- claims processing - getting those bills to the payers
- scheduling - getting patients in the door
- patient billing - getting patient responsibility collected
- eligibility verification - ensuring eventual payment for service provided
These initial automation efforts laid the groundwork for more advanced RCM automation technologies, including AI and machine learning, which are now integrated into more complex RCM processes. Still, healthcare organizations must proceed one step at a time, adding automation solutions as budgets allow.
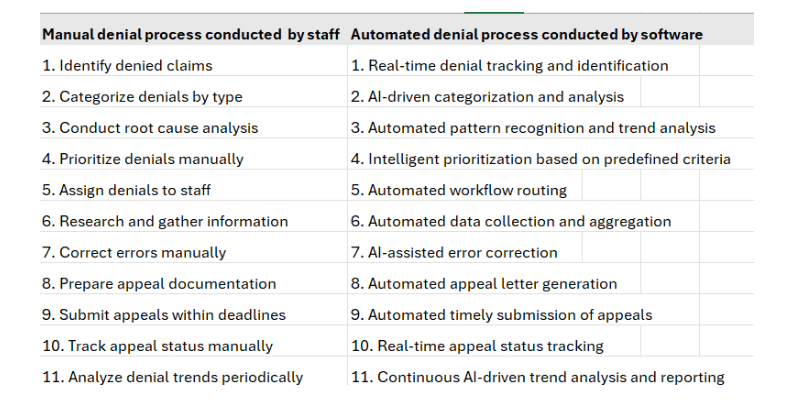
The left column on the table below reveals the 11 steps RCM staff must undertake to get one denial appealed. The right column lists all of the tasks completed by automated denials software. This process relies on data analytics, artificial intelligence, and automated tools to streamline operations and gain insights into denial patterns and trends.
Denial management automation also assembles clear reports that help your team understand the codes and payers triggering costly denials. Root cause identification and trend analysis allow you to prevent denials before they occur.
Take a quick, self-guided tour through a powerful denial and contract management system:
5 reasons a denial management process crucial for MSOs and revenue cycle leaders
A robust denial management process is crucial for Managed Service Organizations (MSOs) and revenue cycle leaders for several key reasons:
1. Revenue impact: Denials significantly impact revenue generation. The American Health Information Management Association (AHIMA) tells us that up to 67% of denials are recoverable. Despite this potential win, if staff time invested outweighs recovery, it's not prioritized. Denial management automation lifts the burden so that the staff time invested becomes negligible and revenue optimized.
Rampant denials, on the other hand, cause delays in payments, potentially leading to uncompensated care. When your staff or automation identifies the CPT codes and payers that trigger denials, you can take steps to submit claims according to more accurate coding or payer requirements. Staff should be on alert to double-check these claims. When they can ensure that all documents are included and no errors appear, denial rates drop. With increased scrutiny from insurers on contract terms and medical necessity, a strong denial management process ensures that documentation is accurate and complete, reducing the risk of denials based on these factors.
2. Prevention of future denials: A comprehensive denial management process involves analyzing root causes and implementing preventive measures. This proactive approach reduces future denials, improving clean claim rates and overall financial performance. When the average cost of claim rework can be up to $25 for ambulatory providers and $118 for hospitals, denial prevention is critical.
3. Operational efficiency: By implementing a data-driven denial management process with clearly defined claim adjustment reason codes (CARCs) and assigned responsibilities, organizations can streamline their workflows and improve overall operational efficiency.
4. Improved Cash Flow: Addressing denials promptly (within 48 hours of receipt) can reduce reimbursement delays by 21-45 days, ensuring better cash flow for the organization. Healthcare organizations need either a fast-responding denial management team or automation to promptly respond. Those looking for an automated software denial management system should insist on real-time visibility capabilities. This function allows you to monitor, analyze, and act upon payer responses as soon as they occur.
5. Adaptation to value-based care: As healthcare transitions to value-based care models, denial management becomes even more complex. An effective process put in place now will help your organization navigate the challenges of attribution and financial reconciliation in these new payment models.
The ideal denial management process: 8 steps
By implementing a structured and comprehensive denial management process, healthcare providers can significantly reduce denial rates, improve cash flow, and optimize financial performance. Your denial management process may be conducted in-house by staff, outsourced to a third party or handled by a combination of staff and automated software (see below).
No matter your approach, the following seven steps outline a robust denial management process that combines insights and proactive measures to address and prevent claim denials.
Now matter how you execute, the denial management process involves the following steps:
1. Identification: Detect and flag denied claims in the billing system. Such categories could include denials related to:
- coding
- pre-authorization
- eligibility
In addition to categorizing the reports, make sure that all information is easily accessible by all staff. If you’re keeping denial management in-house, organize a team to evaluate the reports and set an action plan in place. This team and specific departments should meet on a regular basis and discuss any issues and how to address them.
2. Analysis: Investigate the root causes of denials, categorizing them by type (e.g., coding errors, eligibility issues, missing documentation). Determining the cause for each denial helps prevent future claims. Were there coding mistakes? Lack of prior authorization or documentation? Identifying underlying issues will not only help your business recover losses but will also improve patient satisfaction.
3. Prioritization: Rank denials based on factors such as patient well-being, dollar amount, likelihood of reversal, and payer deadlines.
4. Correction and Resubmission: Address the issues that caused the denial, such as correcting coding errors or updating documentation, and resubmit the claim.
Implement a strategic incentive program to enhance denial management effectiveness. By setting clear deadlines for report completion (typically 5-7 business days) and offering rewards for timely submissions, identifying process improvements, and reducing denial rates, healthcare organizations can boost team productivity and engagement. This approach not only motivates employees to excel in their current roles but also encourages them to contribute to long-term revenue cycle optimization.
5. Appeals: For denials that cannot be resolved through simple corrections, prepare and submit formal appeals to payers within specified timelines.
6. Tracking: Monitor the progress of resubmitted claims and appeals to ensure timely resolution. Set specific, measurable targets for denial reduction and resolution. These may include:
- reducing the overall denial rate by a certain percentage
- improving clean claim rate
- decreasing average days in accounts receivable
- establish clear deadlines for denial reports and resolutions.
7. Recovery: When denials you appeal do not result in an overturn, it takes someone to make contact with the payer to move the process forward and recover this reimbursement.
8. Prevention: Implement process improvements and corrective actions based on denial trends to prevent future occurrences.
9. Reporting and analysis: Regularly review denial data to identify patterns and track key performance indicators (KPIs), such as claim denial rate, first pass resolution rate, and days in accounts receivable (A/R). Keeping tabs on these figures establishes the effectiveness of your denial management efforts. Remember “What gets measured, gets managed” – Peter Drucker’s resonant warning. Consider offering frequent updates on individual and team performance at report time. Share success stories to motivate and inspire other team members.
Regular audits should be conducted to review the denial management process and compare performance against industry standards.
Three denial management system options
The landscape of denial management in healthcare has evolved significantly, offering organizations multiple approaches to tackle this critical aspect of revenue cycle management. Each method presents unique advantages and challenges, catering to different organizational needs, resources, and strategic priorities. Understanding these three primary denial management systems—in-house teams, outsourcing, and software solutions—is crucial for healthcare providers to make informed decisions that align with their operational goals and financial objectives.
1. In-house with an internal team:
This approach involves creating a dedicated team within the organization to handle denial management. It allows for greater control over the process and enables the team to develop deep institutional knowledge. However, it requires investment in staff, training, and technology, and may struggle to scale during peak periods.
2. Outsourced to a third party:
Outsourcing denial management to specialized vendors can provide access to expertise and advanced technologies without the need for large upfront investments. This option can be particularly beneficial for smaller organizations or those facing staffing challenges. However, it may result in less direct control over the process and potential communication challenges.
3. Denial management software
Denial management software automates many aspects of the process, from identifying denials to generating appeals. This approach can significantly increase efficiency and accuracy while providing real-time analytics. However, it requires careful selection of the right software, integration with existing systems, and ongoing maintenance and updates.
We cover all three options here.
Handling denial management in-house
Setting up an in-house denial management team involves 10 key steps:
1. Assemble a dedicated team: Recruit or reassign staff with expertise in medical coding, billing, and clinical knowledge. Include registered nurses or those with case management experience for handling clinical denials.
2. Implement a data-driven process: Develop a structured workflow with clearly assigned responsibilities, utilizing real-time data and analytics to empower the team.
3. Establish a "Cradle to Grave" approach: Assign accounts to team members who handle all aspects of a denial, avoiding splitting work across multiple staff.
4. Create specialized sub-teams: Separate the team into technical and clinical denial specialists to address different types of denials efficiently.
5. Develop standardized templates: Build and maintain a centralized repository of appeal templates tailored to specific payers and denial types.
6. Implement denial management software: Invest in technology that automates identification, categorization, and tracking of denials. Once this technology is in place, it will execute much of the denial management work, freeing and supporting staff.
7. Provide ongoing training: Offer continuous education on coding guidelines, payer policies, and best practices in denial management.
8. Set up performance metrics: Establish KPIs to track the team's effectiveness and identify areas for improvement.
9. Create feedback loops: Implement a system for the denial management team to provide insights to other departments to prevent future denials.
10. Develop a prioritization strategy: Create a workflow that prioritizes denials based on factors like dollar amount and likelihood of overturn.
By following these steps, organizations can create an effective in-house denial management process that leverages institutional knowledge and maintains control.
Outsourcing the denial management process
Outsourcing your denial management process will free your employees to focus on patient care. While these services can be pricy, outsourced denial management teams bring specialized knowledge, including:
- in-depth understanding of payer regulations and industry standards
- knowledge of the most current billing and coding rules
- experience tracking down root causes of denials and developing prevention strategies
Denial management experts contact patients to receive any information needed to resolve claims, such as coordination of benefits, questionnaires, PIP applications, etc. They determine coverage in advance and secure approval for a proposed treatment before services are rendered.
Outsourcing denial management services also promises to:
- streamline processes and reduce time to denial appeals
- use advanced tools to identify trends and patterns in denials
- boost claim approval rates
- reduce billing errors that frustrate patients
- eliminate the need for ongoing staff training
- keep patients informed about their insurance policies and potential out-of-pocket expenses
- secure pre-approvals before services are rendered
- implement strategies to prevent future denials
These improvements can boost the revenue cycle, but they also move the control out of the organization’s hands. Because they involve human specialists, they also can be expensive.
Automated denial management software
Many of the advantages outsourcing offers can be achieved with automated software tools.
Automating the processes involved in denial management does require some staff training and time, but these tasks remain in house, which has some advantages.
AI-driven robotic process automation can:
- quickly identify and categorize denials using machine learning algorithms
- automatically sort denials by type, payer, or root cause
- prioritize denials based on potential revenue impact or time sensitivity
- populate appeals with relevant patient and claim information
- track appeal deadlines and send reminders to staff
- automate repetitive tasks such as data entry and claim status checks
- reduce human error common in routine, tedious processes
- free up staff time for more complex, high-value tasks
- automatically generate appeal letters using predefined templates
- generate real-time dashboards on denial trends and patterns
And it carries out these tasks in minutes, without tiring or getting confused.
Denial management automation strengthens revenue cycle management by significantly reducing human resource hours, enhancing appeal accuracy, and boosting staff productivity. Its key features, including real-time tracking and dashboards, provide immediate visibility into trends and emerging issues, allowing healthcare providers to detect and respond to potential threats before they impact revenue. Comprehensive performance metrics help stakeholders make informed decisions quickly, adapt to changing payer policies, and implement proactive strategies.
By consistently tracking progress, healthcare organizations can pinpoint areas needing improvement, make data-driven refinements, and demonstrate ROI to stakeholders.
This approach not only optimizes denial management but also enhances overall operational efficiency, leading to reduced denial rates and improved financial health. Crucially, it allows healthcare organizations to adapt continuously to evolving healthcare regulations and payer policies, ensuring long-term success in managing denials and optimizing revenue cycles.
Denial management software combined with denial recovery services
While software does shoulder much of the denial management workload, creating appeals and pursuing payers often requires a staff member or outside specialist. Some advanced denial management software companies make recovery experts available to you. These professionals take over communications with payers. They clearly convey your organization’s expectations to help secure what’s rightfully yours. With both advanced software and expert services, you establish an end-to-end denial management process.
Let MD Clarity simplify your denial management process
An effective denial management process is indispensable for healthcare providers seeking to maximize net revenue and maintain financial stability.
MD Clarity’s RevFind digs deep to find the root causes of denials and guides your staff in appealing. Your EHR may have a denials reporting feature, but often, its limited data points fail to diminish your denial rates. A platform for underpayment detection, denial management, and contract optimization, RevFind is built from the ground up to surface, analyze, and report denials.
With RevFind, you can:
- Streamline denial management to reduce administrative burden and speed up cash flow
- View denial opportunities from highest to lowest sorted by payer and CPT code combination
- See which denial reasons cost you the most
- Pinpoint which facilities and physicians generate the most denials
- Track denial recovery as claims move through the appeal process
- Centralize payer contracts for easy tracking and compliance
- Detect underpayments automatically and recover lost revenue
As much work as RevFind conducts, sometimes it takes a staff member to take this information to payers to win appropriate reimbursement. MD Clarity’s denial recovery experts step in to navigate payer red tape and stall tactics. Armed with RevFind’s analytics, they back up all requests with concrete data. This synergy of software and expert services amounts to a seamless, end-to-end solution -- MD Clarity's Denial Recovery Services --that prevents you from having to hire additional staff.
that prevents you from having to hire additional staff.
Get a demo to see how MD Clarity’s RevFind software lowers your denials rate, and revenue recovery services to get payers reimbursing appropriately.
FAQs
Get paid in full by bringing clarity to your revenue cycle



.svg)
.svg)