Effective across the U.S. since Jan. 1, 2022, the No Surprises Act establishes federal protections against surprise medical bills, which occur when consumers receive care from out-of-network doctors, hospitals, and other healthcare providers.
One of the most important parts of the No Surprises Act is the good faith estimates (GFE) provision. This provision requires healthcare providers to make comprehensive GFEs of charges for services and items provided to uninsured patients and self-pay insured patients who do not want to submit claims to their insurers. GFEs are notifications that outline uninsured or self-pay individuals' expected charges for a requested or scheduled service or item. It should include primary services and items as well as items and services reasonably expected to be provided, even if the patient will receive the services and items from another facility or provider.
Read this guide to learn more about the No Surprises Act and good faith estimate requirements. Along the way, we will discuss who must comply with the No Surprises Act's GFE requirements, who receives GFEs, whether you can issue a single estimate for recurring services, time frames for providing GFEs to individuals, rules for changing GFEs, GFE disclosure requirements, GFE regulations for co-providers, and more.
Who Must Comply With Good Faith Estimate Requirements?
Every healthcare provider must comply with the No Surprises Act's GFE requirements. For the purposes of the GFE, a healthcare provider means a physician or another type of provider acting within the practice scope of their certification or license, including providers of air ambulance services.
Additionally, every healthcare institution licensed under applicable local or state law as a healthcare facility must comply with the No Surprises Act's GFE requirements. Examples include:
- Hospitals
- Critical access hospitals
- Federally qualified health centers
- Hospital outpatient departments
- Imaging centers
- Ambulatory surgical centers
- Rural health centers
- Laboratory centers
Who Must Receive a GFE?
Under the No Surprises Act, anyone who is uninsured or decides to pay for their own medical expenses must receive a GFE.
What You Must Ask To Determine Who Receives a GFE
To determine whether someone needs a GFE, ask them whether they are enrolled in:
- A Federal healthcare program
- A group health plan
- An individual or group health insurance coverage offered by a health insurance issuer
- A health benefits plan under a Federal Employees Health Benefits Program
If the individual is not enrolled in any of these, they are considered uninsured, and you must give them a GFE.
If they are enrolled in one of the above, ask them whether they are submitting a claim. If not, the individual is considered self-pay and must receive a GFE.
Can You Issue a Single Estimate for Recurring Services?
Yes, you can issue a single estimate for recurring primary services or items if both of the following requirements are met:
- The scope of a GFE for recurring primary services or items does not exceed 12 months. If additional recurrences of such services and items are expected beyond 12 months, a convening facility or provider must provide a self-pay or uninsured patient with a new GFE and inform them of changes upon delivery of the new GFE.
- The GFE for recurring services or items includes the expected scope of the recurring primary services or items, such as frequency, time frames, and the total number of services and items.
Time Frames for Providing Good Faith Estimates to Individuals
After receiving a GFE request from an uninsured or self-pay individual or scheduling a primary service or item for such an individual, you must contact all co-facilities and co-providers who are reasonably expected to provide services or items in support of or in conjunction with the primary service or item, no later than one business day after receiving or scheduling the request.
Note that you must request the co-facilities and the co-providers to submit GFE information to you. The request should have the date by which you must receive the GFE.
You also need to provide a GFE to an uninsured or self-pay patient within the following time frames:
- When a primary service or item is scheduled at least three business days before the date the service or item is scheduled, you must provide the GFE no later than one business day after the scheduling date.
- When a primary service or item is scheduled at least 10 business days before the furnishing date, you must provide the GFE no later than three days after the scheduling date.
- When an uninsured or self-pay individual requests a GFE, you must provide the GFE no later than three business days after the date of the request.
The U.S. Department of Health and Human Services recognizes that some facilities or providers may need to establish secure and efficient communication channels for sending GFE information between convening facilities or providers and co-facilities and co-providers. HHS also understands that it may take time for facilities and providers to create reliable processes and systems for providing and receiving GFE information from co-facilities and co-providers.
Accordingly, from Jan. 1, 2022, to Dec. 31, 2022, HHS will exercise enforcement discretion when facilities and providers send GFEs to insured or self-pay individuals that do not include expected costs from co-facilities co-providers.
Note that a co-facility or co-provider is not prohibited from furnishing GFE data before Dec. 31, 2022. The self-pay or uninsured individual can separately request a GFE directly from the co-facility or co-provider. In such a case, the co-facility and co-provider would be required to provide the GFE for the services or items.
Generally speaking, the HSS encourages providers and convening facilities to include a range of expected charges for services and items reasonably expected to be billed and provided by co-facilities and co-providers. It also encourages states to take similar approaches and will not consider states to have failed to enforce GFE requirements if they take these approaches from Jan. 1, 2022, through Dec. 31, 2022.
Rules for Changing a Good Faith Estimate
If you or a co-facility or co-provider anticipates or is notified about any changes to the scope of a previously-furnished GFE at the time of scheduling, you must provide the uninsured or self-pay individual with a new GFE no later than one business day before the services or items are scheduled to be furnished.
If any changes in expected facilities or providers in a GFE occur less than one business day before a service or item is scheduled to be furnished, the replacement facility or provider must accept the GFE provided by the former facility and provider.
If the patient is uninsured or self-pay, you must provide them with a new GFE for the scheduled service or item according to the standard time frames in the "Time Frames for Providing Good Faith Estimates to Individuals" section of this guide.
Good Faith Estimate Disclosure Requirements
You must prominently display clear, comprehensive, and easy-to-find information about the availability of GFEs for uninsured or self-pay individuals in your office, on your site, and wherever scheduling and questions about the cost of services and items happen. The GFE information on your site must be easily searchable from a public search engine like Google or Bing. Feel free to use these model notices as references.
You must also provide information about GFEs for uninsured or self-pay individuals when scheduling a service or item or when asked questions about the cost of services or items. You should consider any inquiry or discussion about the potential cost of services or items as a GFE request.
Additionally, you must make information about GFE availability for uninsured or self-pay individuals available in:
- Accessible formats
- The language(s) spoken by the patient(s) considering or scheduling services or items
GFE Regulations for Co-Providers
Co-facilities and co-providers must submit GFE information upon your request. They must provide the GFE information no later than one business day after receiving your request.
Additionally, co-facilities and co-providers must provide new GFE to you if they anticipate any changes to the scope of the GFE information previously submitted. This includes anticipated changes to the expected services, charges, recurrences, items, providers, duration, or facilities.
If any changes to the co-facilities and co-providers listed in the GFE happen less than one business day before the service or item is scheduled to be furnished, the replacement co-facility or provider must accept the GFE for the relevant services and items included in the GFE provided by the replaced facility or provider as its GFE of expected changes.
If a self-pay or uninsured individual separately requests or schedules a GFE from a facility or provider that would otherwise be a co-facility or co-provider, that facility or provider must meet all requirements for GFE-issuing convening facilities and providers.
Content Requirements for Good Faith Estimates Given to Patients by Providers
A GFE issued to a self-pay or uninsured individual must include:
- Patient's name and date of birth
- Description of the primary service or item in understandable and clear language
- The scheduled date of the primary service or item
- A list of the following, grouped by each facility and provider:
- Services and items reasonably expected to be furnished for the primary service or item, including medical tests, encounters, supplies, prescription drugs, durable medical equipment, and facility fees
- Services and items reasonably expected to be furnished along with the primary service or item for that period of care
- Services and items reasonably expected to be furnished by co-facilities and co-providers
- Expected service codes, applicable diagnosis codes, and expected changes associated with each listed service or item
- Service codes identify and describe a service or item using the Healthcare Common Procedure Coding System, Current Procedural Terminology, National Drug Codes, and Diagnosis-Related Group code sets.
- Diagnosis codes use the International Classification of Diseases code set to describe an individual's injury, disease, disorder, or other health conditions.
- Expected changes refer to the cash pay rates established by a facility or provider for a self-pay or uninsured individual. It should reflect relevant discounts.
- Name, Tax Identification Number, and National Provider Identifier of each facility or provider represented in the GFE
- State(s), facility location(s), and office where the services or items are expected to be furnished
- A list of services or items that may require separate scheduling and are expected to happen after or before the anticipated period of care for the primary service or item. The GFE must include a disclaimer directly above this list that includes all of the following:
- A notification that information like service codes, diagnosis codes, expected charges, and facility and provider identifiers do not need to be included for items and services in this list. This information will be provided in separate GFEs upon requesting or scheduling the listed items and services.
- An explanation that separate GFEs will be issued to an uninsured or self-pay individual upon scheduling or requesting the listed services or items.
- Instructions for how an uninsured or self-pay individual can get GFEs for such services or items.
- A disclaimer informing the self-pay or uninsured patient that there may be additional recommended services or items that must be requested or scheduled separately. The disclaimer must remind the patient that these additional services or items are not reflected in the GFE.
- A disclaimer informing the self-pay or uninsured patient that the information in the GFE is only an estimate and that actual charges, items, and services may differ from the GFE
- A disclaimer informing the self-pay or uninsured individual of their right to initiate the Patient-Provider Dispute Resolution process if the actual billed charges are $400 or more than the expected GFE charges. The disclaimer must include instructions for where the patient can find information about how to start the PPDR process. It must also state that initiation of the PPDR process will not negatively affect the quality of health services furnished to the individual by a facility or provider.
- A disclaimer that the GFE is not a contract and does not require the self-pay or uninsured individual to obtain the services or items from any of the facilities or providers identified in the GFE. Use this example disclaimer notice as a reference.
You can use charts like this to list out expected services or items for uninsured or self-pay individuals:
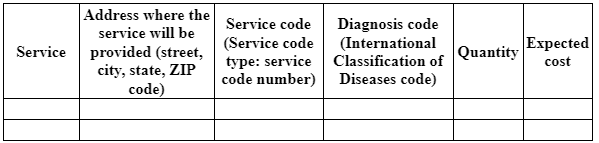
Include the total expected charges and additional notes at the bottom.
Content Requirements for Good Faith Estimates Given to Convening Providers by Co-Providers
GFE information submitted to you by co-providers and co-facilities for inclusion in GFEs must include:
- Patient name and date of birth
- A list of services and items expected to be provided by the co-facility and co-provider that are reasonably expected to be furnished along with the primary service or item as part of the period of care
- Expected service codes, applicable diagnosis codes, and expected charges associated with each listed service or item
- Name, Tax Identification Numbers, and National Provider Identifiers of the co-facility or co-provider
- State(s), facility location(s), and office where the services or items are expected to be furnished by the co-facility or co-provider
- A disclaimer that the GFE is not a contract and doesn't require the self-pay or uninsured individual to obtain the services or items from any of the co-facilities or co-providers identified in the GFE
What Is the Patient-Provider Dispute Resolution Process, and How Does It Work?
Starting Jan. 1, 2022, a PDDR process will be available for self-pay or uninsured patients who receive a bill for a service or item that costs $400 or more than the expected charges on their GFEs.
Under the PPDR process, the self-pay or uninsured individual may request a determination from a Selected Dispute Resolution (SDR) entity for the amount they have to pay. This can give the individual vital consumer protections from charges that are much higher than the expected GFE estimates.
The PPDR process can apply to any service or item furnished by a convening facility, provider, co-facility, or co-provider to a self-pay or uninsured individual where the total billed charges are $400 or more than the GFE amounts.
If a co-facility or a co-provider that provided a GFE service or item estimate is replaced by another co-facility or co-provider less than one business day before that service or item is scheduled to be furnished, that item or service is eligible for dispute resolution if the billed charge is $400 or more than the total expected GFE charges.
If the replacement facility or provider provides the self-pay or uninsured individual with a new GFE on time, the item or service is only eligible for dispute resolution if the total billed charge for the replacement co-facility or co-provider is $400 or more than the total expected charges in the replacement co-facility or co-provider's GFE.
Can a Facility or Provider Be Subject to PPDR Requirements But Not GFE Requirements?
GFE and PPDR requirements work together to establish key consumer protections for self-pay or uninsured individuals who receive medical bills that are $400 or more than their GFEs. PPDR requirements apply to all facilities and providers subject to GFE requirements.
Can Facilities and Providers Settle Their Payment Disputes With Self-Paying and Uninsured Individuals During PPDR?
Yes. Providers and facilities can settle their payment disputes through the PPDR. HHS recognizes both parties have a right to resolve disputes through the PPDR process.
After the PPDR process has started but before the date of the SDR's determination, both parties can settle the payment amount through:
- An offer to accept a lower amount
- An agreement by the self-paying or uninsured individual to pay the charges in full
- An offer of financial assistance
Required Mediums for Good Faith Estimates
A GFE must be provided within the time frames described above in written form, either electronically or on paper, depending on the self-pay or uninsured patient's preferences. Electronically-provided GFEs must be provided in a manner that the self-pay or uninsured individual can both print and save. Meanwhile, GFEs provided to self-pay or uninsured patients through paper mail must be postmarked by the timelines in the "Time Frames for Providing Good Faith Estimates to Individuals" section.
If an uninsured or self-pay individual requests a GFE in a form other than electronic or paper, such as orally or by phone, you may orally inform the individual of the information in the GFE using the requested method. However, you must also issue the GFE to the uninsured or self-pay individual in written form to meet the requirements of this section.
Other Requirements and Gotchas
Additional GFE requirements and gotchas include:
GFEs as Part of Patients' Medical Records
A GFE issued to a self-pay or uninsured individual is considered part of the patient's medical record. Accordingly, you must maintain it like a patient's medical record. As a convening facility or provider, you must also provide a copy of any previously issued GFE furnished within the last six years to a self-pay or uninsured individual upon the individual's request.
Consequences of Making Errors or Omissions in GFEs
Note that you will not fail to comply with federal GFE requirements solely because you have made an omission or error in a GFE, provided that you correct the information as soon as possible. If services and items are furnished before a GFE error is addressed, you may be subject to PPDR if the actual billed charges are "substantially in excess" of the amounts in the GFE. HHS regulations define "substantially in excess" as $400 or more above the GFE amounts.
Similarly, you are not failing to comply with federal GFE requirements if you rely on information from another provider or facility to obtain information from another individual or entity unless you know or reasonably should have known that the information is inaccurate or incomplete. If you discover the information is incomplete or inaccurate, you must provide corrected data to the uninsured or self-pay individual as soon as possible. If the services or items are furnished before you can address the GFE error and the actual billed charges are $400 or more than the GFE amounts, you may be subject to PPDR.
Follow the No Surprises Act's GFE Requirements
As you can see, the No Surprises Act establishes strict guidelines for creating and sending GFEs.
Specifically, you must:
1. Determine whether someone needs a GFE.
2. If certain requirements are met, issue a single estimate for recurring items or services.
3. Provide GFEs according to No Surprises Act time frames.
4. Provide the self-paying or uninsured individual with a new GFE no later than a business day if you anticipate or are notified about any changes to previous GFEs.
5. Display prominent notices about the availability of GFEs for uninsured and self-paying individuals.
6. Get co-providers and co-facilities to submit GFE information within one business day after your request.
7. Include the right content in your GFEs.
8. Participate in the PPDR process as needed.
9. Provide GFEs in paper or electronic form.
10. Consider GFEs part of patients' medical records.
11. Correct omissions and errors as soon as possible.
If you don't follow the No Surprises Act requirements, you may be subject to civil monetary penalties of up to $10,000.
Get paid in full by bringing clarity to your revenue cycle


.avif)
.svg)
.svg)
.avif)

