With 2023 fast approaching, you'll soon be required to use Version 2 of the No Surprises Act notice and consent form. We offer you a compact guide to Version 2, including the most frequently asked questions on the topic, and a detailed walk-through of how to use it.
{{toc}}
No Surprises Act Notice and Consent FAQ
Here are some answers to the most frequently asked questions about the No Surprises Act notice and consent form:
What is the purpose of the notice and consent form?
The notice and consent form is designed to protect insured patients from unexpected medical charges as a result of balance billing for out-of-network services.
Who must receive the No Surprises Act consent form?
The No Surprises Act consent form must be provided to insured patients using out-of-network or non-participating providers. These patients may be insured either privately or under employer-provided health plans.
Ineligible patients include the following:
- Uninsured patients
- Patients on Medicare or Medicaid
- Patients seeking services only from in-network providers
What types of providers are required to provide notice?
There are three types of providers required to provide notice:
- Ambulatory surgery centers
- Hospitals
- Individual providers
Why are there two versions of the consent form, and which one do I use?
Version 1 of the consent form is only meant to be used in 2022, while Version 2 is for use during 2022 and beyond. The largest difference between the two versions is the information that must be included in the Good Faith Estimate (GFE). Starting in 2023, the GFE must reflect information from co-providers and co-facilities. Version 2 includes a section prompting providers to supply these details.
How do you provide the notice?
When delivering the notice to the patient, you must follow these requirements:
- The notice must be provided separately and not bundled in with other documents.
- A representative from the provider should be available in person or via phone to explain the consent form and estimates, and to answer the patient's questions.
- You must provide the form on paper unless the patient requested an electronic form.
- The patient must receive a copy of the signed notice in person, by mail, or by email if requested.
- The documents must meet any applicable language access requirements as stated in 45 CFR 149.420.
- You must translate the documents or provide a qualified interpreter, if required.
When must you provide the notice?
The deadline for providing the notice depends on how far in advance the patient schedules their appointment.
Appointments scheduled 72+ hours in advance
If the appointment is scheduled at least 72 hours in advance, you must provide these notice and consent papers at least 72 hours before the scheduled service. You must provide these papers to the patient or their authorized representative.
Appointments scheduled less than 72 hours in advance
If the appointment is scheduled less than 72 hours in advance, you must provide the notice and consent papers to the patient or their authorized representative on the day of the appointment. In these situations, however, you must deliver the papers at least three hours before the appointment.
Do you have to provide the notice every single time?
Yes, you must provide the notice every time without exception.
Can you modify the consent form?
No, you are not permitted to modify the consent form. Exceptions include to follow the instructions within the form, or to follow state law. The bracketed, or bracketed and italicized, text serves as instructions within the form template. It should be deleted before giving the consent form to the patient.
No Surprises Act Model Notice
Both Versions 1 and 2 of the No Surprises Act notice and consent form are available online. You can download them directly from the Centers for Medicare & Medicaid Services.
Surprise Billing Protection Form Walk-Through
Due to the limited utility of Version 1, this walk-through focuses solely on Version 2. It is essential to remember that you must delete the italicized instructions in brackets prior to providing the notice to the patient.
Surprise Billing Protection Form Overview

Page One provides an introduction and gives the patient basic information about the Surprise Billing Protection Form. This page includes the following:
- The purpose of the form
- An alert that patients are not required to sign the form and should not sign it in certain situations
- Guidance that patients can ask their provider or patient advocate for assistance with the form
- A notice that receiving care from this provider will likely cost more because it isn't in the patient's health plan network
- A notice that the patient is protected under federal law from higher medical bills in certain situations, and information about who they can speak to about these protections
- A notice that the patient may pay more if they sign the form
You must provide this page of the Surprise Billing Protection Form to the patent, but there is nothing to fill out or delete on this page.
Total Cost Estimate and Information About Rights and Protections
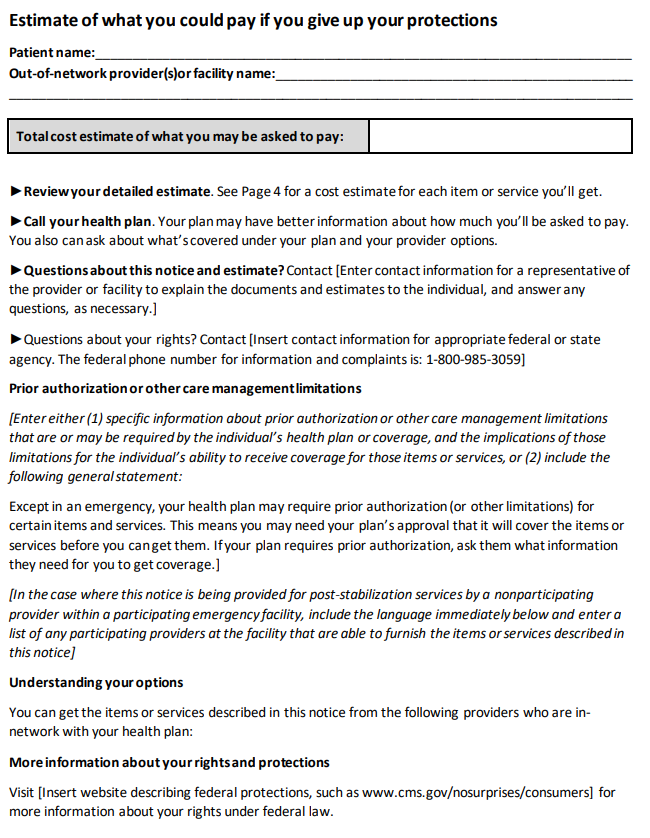
Page Two includes the patient's name, the provider or facility's name, and the total estimated cost. This page also includes the following information:
- Where patients can view a cost estimate for each included item or service (Page 4)
- Guidance to call their health plan for more information about what the patient should expect to pay
- Contact information for a representative who can explain the document and cost estimates, and answer the patient's questions
- Either specific care management or prior authorization limitations, or a general statement
- A list of in-network health plan providers who can offer the same item or service
- Website information where the patient can obtain more information about their federal rights
Page Two of the form requires you to fill in a substantial amount of information in the following order:
- List the patient's full name.
- List the name of the out-of-network facility or provider.
- List the total cost estimate the patient is currently expected to pay. This will be the total estimate from the Good Faith Estimate on the last page of the notice.
- Under the third bullet point, "Questions about this notice and estimate," enter the contact information for the provider or facility's representative who the patient can contact with questions about the estimate and notice.
- Under the fourth bullet point, "Questions about your rights," insert the contact information for the appropriate state or federal agency.
- Under the section "Prior authorization or other care management limitations," choose one of two options: Either (1) enter specific information about the prior authorization or other limitations that may be required by the patient's health plan coverage and the impact of those limitations on the patient receiving coverage, or (2) include a pre-written general statement.
- Under the section "Understanding your options," you must list the in-network providers who can provide the patient's desired services or items without triggering the higher out-of-network charges.
Under the final section, you must insert a website that describes the patient's federal protections. An example of an acceptable website is: www.cms.gov/nosurprises/consumers.
Signature Page

The third page of the document also requires personalization. The following items require you to add or delete information:
- Where the form says, "[doctor's or provider's name...]," you must create a separate check box for each applicable doctor or provider if there are multiple. Next to each checkbox, list the doctor's or provider's full name.
- Under the third bullet point, enter the "date of notice." This is the date the patient receives the notice from you.
- The patient must fill out the patient signature area at the bottom of the third page, but there is nothing for you to customize here.
Good Faith Estimate

This fourth and final page of the document will also require individualization. The following items require your attention:
- Fill in the patient's name.
- Enter the name of the facility or out-of-network provider.
- In the provided table, enter an itemized list of items and services that you expect to provide. You may add rows if necessary. Include:
- Date of service
- Name of provider or facility
- Service code
- Description of the service
- Estimated amount to be billed for each item or service
- For multiple facilities or providers: Group services and items from the same facility or provider together in adjacent rows. Add a row with the subtotal for each of the facilities or providers.
- For one facility or provider: You may omit the subtotal on page four, however, the total amount from page two must equal the "total estimate of what you may owe."
- Enter the total estimate of what the patient may owe. This is the sum of all items and services across the listed facilities and providers.
The fourth page is critical to complete accurately, as it contains the patient's itemized GFE. The final rules relating to GFEs and AEOBs for insured patients are still pending, but you should stay on the safe side and present accurate estimates.
Remember to delete the instructions in the brackets from each page before delivering the form to the patient.
FAQs
Get paid in full by bringing clarity to your revenue cycle


.avif)
.svg)
.svg)


