


MD Clarity Helps a Major Radiology Practice Improve Collections and Patient Experience
Summary
Challenges
- Ineffective manual benefits checks and payment estimates workflows
- Insufficient number of patient payment estimates provided
- No process in place to accurately collect payment at the point of service
- Frustrated patients
- Extended back-end-weighted revenue cycle
Results
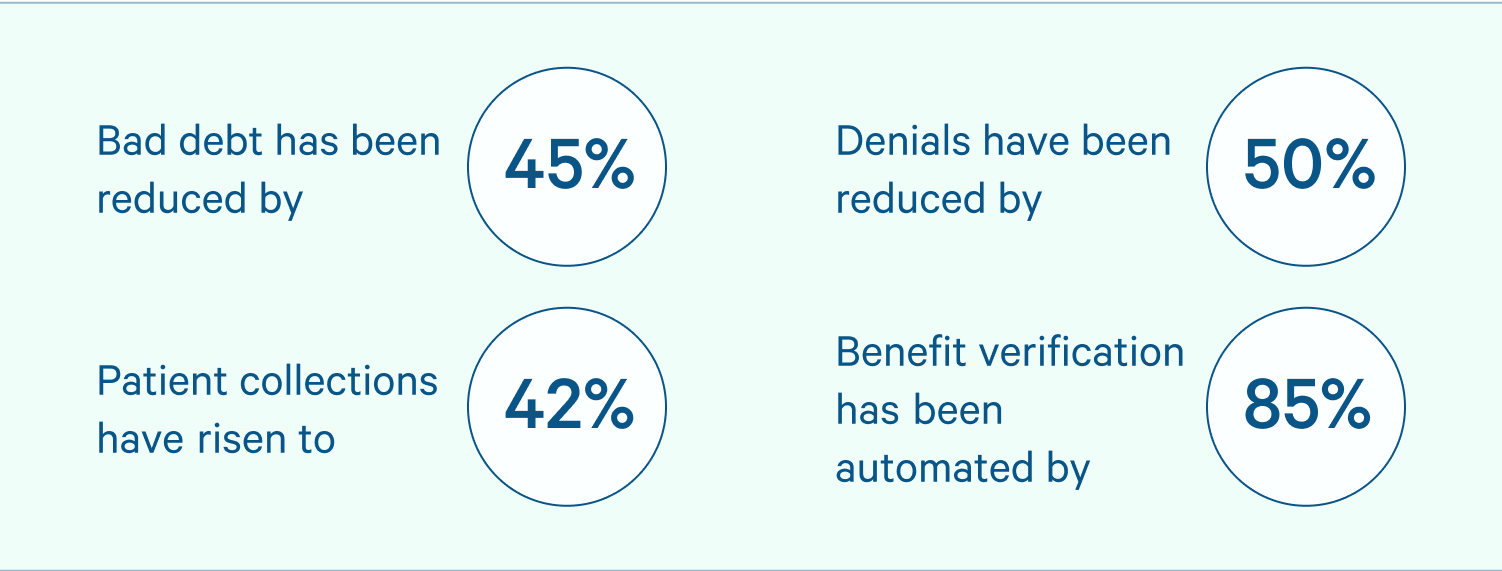
- 45% reduction in bad debt
- 50% reduction in denials
- upfront patient collections increase 42%
- 85% of patient verifications now automated
- RCM staff workload reduced
The Situation: With 200 patients per day, manual eligibility verification and estimates processes lag practice needs
High deductible plans and complex payer networks have put an increased strain on clinical operations, revenue cycle workflows, and the patient experience at a growing radiology practice in the Pacific Northwest. With an average volume of over 200 patients a day, staff simply cannot keep up with manual processes related to checking benefits and providing cost estimates to patients.
Patients get frustrated not knowing the cost of service beforehand, and the practice has found it challenging to quickly and accurately provide this information. This makes it difficult to collect patient fees up front, leading to a back-end-weighted revenue cycle that is complicated and lengthy.
“High deductible plans and complex payer network shave put an increased strain on clinical operations, revenue cycle workflows, and the patient experience." - Business Office Director
The Solution: Clarity Flow automatically detects benefits information and provides price transparency to patients, improving collections
The practice began searching for a solution that could provide extremely accurate estimates to patients prior to procedures. The practice quickly found that MD Clarity’s software was the only one that met the practice's exacting specifications.
- Today, each patient is provided an accurate estimate of their financial responsibility before a procedure is performed. Armed with MD Clarity’s proprietary pricing engine, the practice’s insurance specialists are able to automatically determine allowed amounts in real time, accounting for CMS and payer rules, facility structure, and complex adjustments.
- The Clarity Flow module has been implemented to capture key patient benefit information on the front-end, allowing the practice to find errors that could lead to delayed reimbursement or denials before they happen.
- MD Clarity’s workflow by exception was implemented, which automates the majority of the verification process and only flags patients with insurance issues for staff follow-up. Today, over 85% of patient’s verifications are automated.
- The combination of MD Clarity’s pricing engine, ClarityFlow module, and reporting features gives managers access to the data they need to make better decisions for the practice, and ensure the practice gets paid faster.
Results: Patients appreciate accurate estimates, upfront collections increase, and bad debt and denials shrink
The implementation of MD Clarity’s solutions has been a huge success. Patients love having a clear picture of their financial responsibility. Staff enjoy the increased automation, reducing their manual tasks by 85%. The practice has seen a dramatic reduction in bad debt and an increase in patient collections.

“From day one, it went much easier than staff anticipated,” said the Patient Accounts Manager “Patients really appreciated knowing what they owed before going into the service." - Patients Accounts Manager
The Metrics
The practice began searching for a solution that could provide extremely accurate estimates to patients, prior to their procedures. Ultimately MD Clarity’s solution best met their needs.
.png)
.png)
.png)

.png)



